Gastrointestinal Carcinoid Tumors
Gastrointestinal Neuroendocrine Tumors Treatment (PDQ®)–Patient Version
General Information About Gastrointestinal Neuroendocrine Tumors
Key Points
- A gastrointestinal neuroendocrine tumor is cancer that forms in the lining of the gastrointestinal tract.
- Health history can affect the risk of GI neuroendocrine tumors.
- Some GI neuroendocrine tumors have no signs or symptoms in the early stages.
- Carcinoid syndrome may occur if the tumor spreads to the liver or other parts of the body.
- Imaging studies and tests that examine the blood and urine are used to diagnose GI neuroendocrine tumors.
- Certain factors affect prognosis (chance of recovery) and treatment options.
A gastrointestinal neuroendocrine tumor is cancer that forms in the lining of the gastrointestinal tract.
The gastrointestinal (GI) tract is part of the body's digestive system, a series of hollow, muscular organs joined in a long, twisting tube from the mouth to the anus. The digestive tract processes nutrients in foods that are eaten and helps pass waste material out of the body:
- Food moves from the throat to the stomach through a tube called the esophagus.
- After food enters the stomach, it is broken down by stomach muscles that mix the food and liquid with digestive juices.
- After leaving the stomach, partly digested food passes into the small intestine and then into the large intestine.
- The end of the large intestine, called the rectum, stores the waste from the digested food until it is pushed out of the anus during a bowel movement.
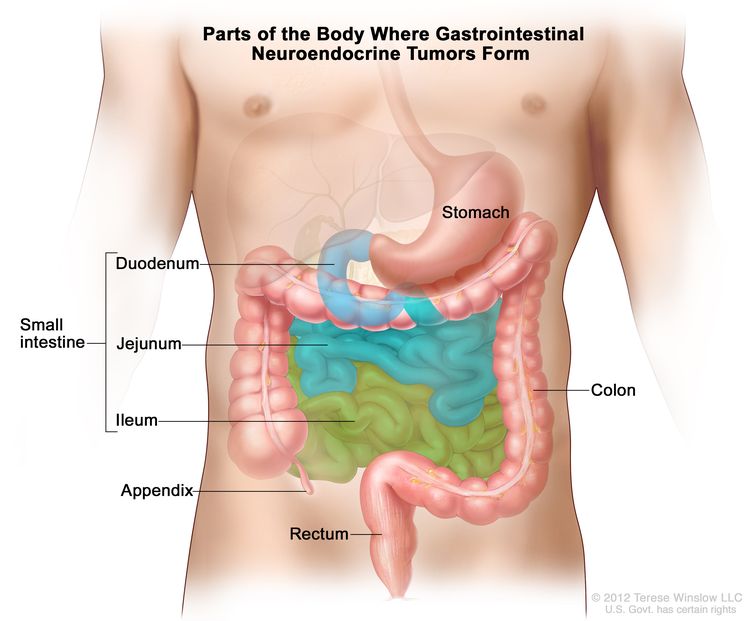
Gastrointestinal (GI) neuroendocrine tumors (also called gastrointestinal carcinoid tumors) form from a certain type of neuroendocrine cell (a type of cell that is like a nerve cell and a hormone-making cell). These cells are scattered throughout the chest and abdomen but most are found in the GI tract. Neuroendocrine cells make hormones that help control digestive juices and the muscles used in moving food through the stomach and intestines. A GI neuroendocrine tumor may also make hormones and release them into the body.
GI neuroendocrine tumors are rare and most grow very slowly. Most of them occur in the small intestine, rectum, and appendix. Sometimes more than one tumor will form.
See the following for information about other types of neuroendocrine tumors:
Health history can affect the risk of GI neuroendocrine tumors.
Anything that increases a person's chance of getting a disease is called a risk factor. Not every person with one or more of these risk factors will develop GI neuroendocrine tumors, and they can develop in people who don't have any known risk factors. Talk to your doctor if you think you may be at risk.
Risk factors for GI neuroendocrine tumors include the following:
- Having a family history of multiple endocrine neoplasia type 1 (MEN1) syndrome or neurofibromatosis type 1 (NF1) syndrome.
- Having certain conditions that affect the stomach's ability to make stomach acid, such as atrophic gastritis, pernicious anemia, or Zollinger-Ellison syndrome.
Some GI neuroendocrine tumors have no signs or symptoms in the early stages.
Signs and symptoms may be caused by the growth of the tumor and/or the hormones the tumor makes. Some tumors, especially tumors of the stomach or appendix, may not cause signs or symptoms. Neuroendocrine tumors are often found during tests or treatments for other conditions.
Neuroendocrine tumors in the small intestine (duodenum, jejunum, and ileum), colon, and rectum sometimes cause signs or symptoms as they grow or because of the hormones they make. Other conditions may cause the same signs or symptoms. Check with your doctor if you have any of the following:
- Duodenum
Signs and symptoms of GI neuroendocrine tumors in the duodenum (first part of the small intestine, that connects to the stomach) may include the following:
- Jejunum and ileum
Signs and symptoms of GI neuroendocrine tumors in the jejunum (middle part of the small intestine) and ileum (last part of the small intestine, that connects to the colon) may include the following:
- Colon
Signs and symptoms of GI neuroendocrine tumors in the colon may include the following:
- Abdominal pain.
- Weight loss for no known reason.
- Rectum
Signs and symptoms of GI neuroendocrine tumors in the rectum may include the following:
- Blood in the stool.
- Pain in the rectum.
- Constipation.
Carcinoid syndrome may occur if the tumor spreads to the liver or other parts of the body.
The hormones made by GI neuroendocrine tumors are usually destroyed by liver enzymes in the blood. If the tumor has spread to the liver and the liver enzymes cannot destroy the extra hormones made by the tumor, high amounts of these hormones may remain in the body and cause carcinoid syndrome. This can also happen if tumor cells enter the blood. Signs and symptoms of carcinoid syndrome include the following:
- Redness or a feeling of warmth in the face and neck.
- Abdominal pain.
- Feeling bloated.
- Diarrhea.
- Wheezing or other trouble breathing.
- Fast heartbeat.
These signs and symptoms may be caused by GI neuroendocrine tumors or by other conditions. Talk to your doctor if you have any of these signs or symptoms.
Imaging studies and tests that examine the blood and urine are used to diagnose GI neuroendocrine tumors.
In addition to asking about your personal and family health history and doing a physical exam, your doctor may perform the following tests and procedures:
- Blood chemistry studies: A procedure in which a blood sample is checked to measure the amounts of certain substances, such as hormones, released into the blood by organs and tissues in the body. An unusual (higher or lower than normal) amount of a substance can be a sign of disease. The blood sample is checked to see if it contains a hormone produced by neuroendocrine tumors. This test is used to help diagnose carcinoid syndrome.
- Tumor marker test: A procedure in which a sample of blood, urine, or tissue is checked to measure the amounts of certain substances, such as chromogranin A, made by organs, tissues, or tumor cells in the body. Chromogranin A is a tumor marker. It has been linked to neuroendocrine tumors when found in increased levels in the body.
- Twenty-four-hour urine test: A test in which urine is collected for 24 hours to measure the amounts of certain substances, such as 5-HIAA or serotonin (hormone). An unusual (higher or lower than normal) amount of a substance can be a sign of disease in the organ or tissue that makes it. This test is used to help diagnose carcinoid syndrome.
- MIBG scan: A procedure used to find neuroendocrine tumors. A very small amount of radioactive material called MIBG (metaiodobenzylguanidine) is injected into a vein and travels through the bloodstream. Neuroendocrine tumors take up the radioactive material and are detected by a device that measures radiation.
- CT scan (CAT scan): A procedure that makes a series of detailed pictures of areas inside the body, taken from different angles. The pictures are made by a computer linked to an x-ray machine. A dye may be injected into a vein or swallowed to help the organs or tissues show up more clearly. This procedure is also called computed tomography, computerized tomography, or computerized axial tomography.
- MRI (magnetic resonance imaging): A procedure that uses a magnet, radio waves, and a computer to make a series of detailed pictures of areas inside the body. This procedure is also called nuclear magnetic resonance imaging
- PET scan (positron emission tomography scan): A procedure to find malignant tumor cells in the body. A small amount of radioactive glucose (sugar) is injected into a vein. The PET scanner rotates around the body and makes a picture of where glucose is being used in the body. Malignant tumor cells show up brighter in the picture because they are more active and take up more glucose than normal cells.
- Endoscopic ultrasound (EUS): A procedure in which an endoscope is inserted into the body, usually through the mouth or rectum. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. A probe at the end of the endoscope is used to bounce high-energy sound waves (ultrasound) off internal tissues or organs, such as the stomach, small intestine, colon, or rectum, and make echoes. The echoes form a picture of body tissues called a sonogram. This procedure is also called endosonography.
- Upper endoscopy: A procedure to look at organs and tissues inside the body to check for abnormal areas. An endoscope is inserted through the mouth and passed through the esophagus into the stomach. Sometimes the endoscope also is passed from the stomach into the small intestine. An endoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove tissue or lymph node samples, which are checked under a microscope for signs of disease.
- Colonoscopy: A procedure to look inside the rectum and colon for polyps, abnormal areas, or cancer. A colonoscope is inserted through the rectum into the colon. A colonoscope is a thin, tube-like instrument with a light and a lens for viewing. It may also have a tool to remove polyps or tissue samples, which are checked under a microscope for signs of cancer.
- Capsule endoscopy: A procedure used to see all of the small intestine. The patient swallows a capsule that contains a tiny camera. As the capsule moves through the gastrointestinal tract, the camera takes pictures and sends them to a receiver worn on the outside of the body.
- Biopsy: The removal of cells or tissues so they can be viewed under a microscope to check for signs of cancer. Tissue samples may be taken during endoscopy and colonoscopy.
Certain factors affect prognosis (chance of recovery) and treatment options.
The prognosis and treatment options depend on the following:
- Where the tumor is in the gastrointestinal tract.
- The size of the tumor.
- Whether the cancer has spread from the stomach and intestines to other parts of the body, such as the liver or lymph nodes.
- Whether the patient has carcinoid syndrome or has carcinoid heart syndrome.
- Whether the cancer can be completely removed by surgery.
- Whether the cancer is newly diagnosed or has recurred.
Stages of Gastrointestinal Neuroendocrine Tumors
Key Points
- After a gastrointestinal neuroendocrine tumor has been diagnosed, tests are done to find out if cancer cells have spread within the stomach and intestines or to other parts of the body.
- There are three ways that cancer spreads in the body.
- Cancer may spread from where it began to other parts of the body.
- The plan for cancer treatment depends on where the neuroendocrine tumor is found and whether it can be removed by surgery.
After a gastrointestinal neuroendocrine tumor has been diagnosed, tests are done to find out if cancer cells have spread within the stomach and intestines or to other parts of the body.
Staging is the process used to find out how far the cancer has spread. The information gathered from the staging process determines the stage of the disease. The results of tests and procedures used to diagnose gastrointestinal (GI) neuroendocrine tumors may also be used for staging. See the General Information section for a description of these tests and procedures. A bone scan may be done to check if there are rapidly dividing cells, such as cancer cells, in the bone. A very small amount of radioactive material is injected into a vein and travels through the bloodstream. The radioactive material collects in the bones with cancer and is detected by a scanner.
There are three ways that cancer spreads in the body.
Cancer can spread through tissue, the lymph system, and the blood:
- Tissue. The cancer spreads from where it began by growing into nearby areas.
- Lymph system. The cancer spreads from where it began by getting into the lymph system. The cancer travels through the lymph vessels to other parts of the body.
- Blood. The cancer spreads from where it began by getting into the blood. The cancer travels through the blood vessels to other parts of the body.
Cancer may spread from where it began to other parts of the body.
When cancer spreads to another part of the body, it is called metastasis. Cancer cells break away from where they began (the primary tumor) and travel through the lymph system or blood.
- Lymph system. The cancer gets into the lymph system, travels through the lymph vessels, and forms a tumor (metastatic tumor) in another part of the body.
- Blood. The cancer gets into the blood, travels through the blood vessels, and forms a tumor (metastatic tumor) in another part of the body.
The metastatic tumor is the same type of tumor as the primary tumor. For example, if a GI neuroendocrine tumor spreads to the liver, the tumor cells in the liver are actually GI neuroendocrine tumor cells. The disease is metastatic GI neuroendocrine tumor, not liver cancer.
The plan for cancer treatment depends on where the neuroendocrine tumor is found and whether it can be removed by surgery.
For many cancers it is important to know the stage of the cancer in order to plan treatment. However, the treatment of GI neuroendocrine tumors is not based on the stage of the cancer. Treatment depends mainly on whether the tumor can be removed by surgery and if the tumor has spread.
Treatment is based on whether the tumor:
- Can be completely removed by surgery.
- Has spread to other parts of the body.
- Has come back after treatment. The tumor may come back in the stomach or intestines or in other parts of the body.
- Has not gotten better with treatment.
Treatment Option Overview
Key Points
- There are different types of treatment for patients with gastrointestinal neuroendocrine tumors.
- The following types of treatment are used:
- Surgery
- Radiation therapy
- Chemotherapy
- Hormone therapy
- Treatment for carcinoid syndrome may also be needed.
- New types of treatment are being tested in clinical trials.
- Targeted therapy
- Treatment for gastrointestinal neuroendocrine tumors may cause side effects.
- Patients may want to think about taking part in a clinical trial.
- Patients can enter clinical trials before, during, or after starting their cancer treatment.
- Follow-up tests may be needed.
There are different types of treatment for patients with gastrointestinal neuroendocrine tumors.
Different types of treatment are available for patients with gastrointestinal neuroendocrine (GI) tumors. Some treatments are standard (the currently used treatment), and some are being tested in clinical trials. A treatment clinical trial is a research study meant to help improve current treatments or obtain information on new treatments for patients with cancer. When clinical trials show that a new treatment is better than the standard treatment, the new treatment may become the standard treatment. Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
The following types of treatment are used:
Surgery
Treatment of GI neuroendocrine tumors usually includes surgery. One of the following surgical procedures may be used:
- Endoscopic resection: Surgery to remove a small tumor that is on the inside lining of the GI tract. An endoscope is inserted through the mouth and passed through the esophagus to the stomach and sometimes, the duodenum. An endoscope is a thin, tube-like instrument with a light, a lens for viewing, and a tool for removing tumor tissue.
- Local excision: Surgery to remove the tumor and a small amount of normal tissue around it.
- Resection: Surgery to remove part or all of the organ that contains cancer. Nearby lymph nodes may also be removed.
- Cryosurgery: A treatment that uses an instrument to freeze and destroy the tumor. This type of treatment is also called cryotherapy. The doctor may use ultrasound to guide the instrument.
- Radiofrequency ablation: The use of a special probe with tiny electrodes that release high-energy radio waves (similar to microwaves) that kill cancer cells. The probe may be inserted through the skin or through an incision (cut) in the abdomen.
- Liver transplant: Surgery to remove the whole liver and replace it with a healthy donated liver.
- Hepatic artery embolization: A procedure to embolize (block) the hepatic artery, which is the main blood vessel that brings blood into the liver. Blocking the flow of blood to the liver helps kill cancer cells growing there.
Radiation therapy
Radiation therapy is a cancer treatment that uses high-energy x-rays or other types of radiation to kill cancer cells or keep them from growing. There are two types of radiation therapy:
- External radiation therapy uses a machine outside the body to send radiation toward the area of the body with cancer.
- Internal radiation therapy uses a radioactive substance sealed in needles, seeds, wires, or catheters that are placed directly into or near the cancer.
Radiopharmaceutical therapy is a type of internal radiation therapy. Radiation is given to the tumor using a drug that has a radioactive substance, such as iodine I 131, attached to it. The radioactive substance kills the tumor cells.
External and internal radiation therapy are used to treat GI neuroendocrine tumors that have spread to other parts of the body.
Chemotherapy
Chemotherapy is a cancer treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing. When chemotherapy is taken by mouth or injected into a vein or muscle, the drugs enter the bloodstream and can reach cancer cells throughout the body (systemic chemotherapy). When chemotherapy is placed directly into the cerebrospinal fluid, an organ, or a body cavity such as the abdomen, the drugs mainly affect cancer cells in those areas (regional chemotherapy).
Chemoembolization of the hepatic artery is a type of regional chemotherapy that may be used to treat a GI neuroendocrine tumor that has spread to the liver. The anticancer drug is injected into the hepatic artery through a catheter (thin tube). The drug is mixed with a substance that embolizes (blocks) the artery, and cuts off blood flow to the tumor. Most of the anticancer drug is trapped near the tumor and only a small amount of the drug reaches other parts of the body. The blockage may be temporary or permanent, depending on the substance used to block the artery. The tumor is prevented from getting the oxygen and nutrients it needs to grow. The liver continues to receive blood from the hepatic portal vein, which carries blood from the stomach and intestine.
The way the chemotherapy is given depends on the type and stage of the cancer being treated.
Hormone therapy
Hormone therapy with a somatostatin analog is a treatment that stops extra hormones from being made. GI neuroendocrine tumors are treated with octreotide or lanreotide which are injected under the skin or into the muscle. Octreotide and lanreotide may also have a small effect on stopping tumor growth.
Treatment for carcinoid syndrome may also be needed.
Treatment of carcinoid syndrome may include the following:
- Hormone therapy with a somatostatin analog stops extra hormones from being made. Carcinoid syndrome is treated with octreotide or lanreotide to lessen flushing and diarrhea. Octreotide and lanreotide may also help slow tumor growth.
- Interferon therapy stimulates the body’s immune system to work better and lessens flushing and diarrhea. Interferon may also help slow tumor growth.
- Taking medicine for diarrhea.
- Taking medicine for skin rashes.
- Taking medicine to breathe easier.
- Taking medicine before having anesthesia for a medical procedure.
Other ways to help treat carcinoid syndrome include avoiding things that cause flushing or difficulty breathing such as alcohol, nuts, certain cheeses and foods with capsaicin, such as chili peppers. Avoiding stressful situations and certain types of physical activity can also help treat carcinoid syndrome.
For some patients with carcinoid heart syndrome, a heart valve replacement may be done.
New types of treatment are being tested in clinical trials.
This summary section describes treatments that are being studied in clinical trials. It may not mention every new treatment being studied. Information about clinical trials is available from the NCI website.
Targeted therapy
Targeted therapy is a type of treatment that uses drugs or other substances to identify and attack specific cancer cells. Several types of targeted therapy are being studied in the treatment of GI neuroendocrine tumors.
Treatment for gastrointestinal neuroendocrine tumors may cause side effects.
For information about side effects caused by treatment for cancer, visit our Side Effects page.
Patients may want to think about taking part in a clinical trial.
For some patients, taking part in a clinical trial may be the best treatment choice. Clinical trials are part of the cancer research process. Clinical trials are done to find out if new cancer treatments are safe and effective or better than the standard treatment.
Many of today's standard treatments for cancer are based on earlier clinical trials. Patients who take part in a clinical trial may receive the standard treatment or be among the first to receive a new treatment.
Patients who take part in clinical trials also help improve the way cancer will be treated in the future. Even when clinical trials do not lead to effective new treatments, they often answer important questions and help move research forward.
Patients can enter clinical trials before, during, or after starting their cancer treatment.
Some clinical trials only include patients who have not yet received treatment. Other trials test treatments for patients whose cancer has not gotten better. There are also clinical trials that test new ways to stop cancer from recurring (coming back) or reduce the side effects of cancer treatment.
Clinical trials are taking place in many parts of the country. Information about clinical trials supported by NCI can be found on NCI’s clinical trials search webpage. Clinical trials supported by other organizations can be found on the ClinicalTrials.gov website.
Follow-up tests may be needed.
As you go through treatment, you will have follow-up tests or check-ups. Some tests that were done to diagnose or stage the cancer may be repeated to see how well the treatment is working. Decisions about whether to continue, change, or stop treatment may be based on the results of these tests.
Some of the tests will continue to be done from time to time after treatment has ended. The results of these tests can show if your condition has changed or if the cancer has recurred (come back).
Treatment of Neuroendocrine Tumors in the Stomach
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of gastrointestinal (GI) neuroendocrine tumors in the stomach may include the following:
- Endoscopic surgery (resection) for small tumors.
- Surgery (resection) to remove part or all of the stomach. Nearby lymph nodes for larger tumors, tumors that grow deep into the stomach wall, or tumors that are growing and spreading quickly may also be removed.
For patients with GI neuroendocrine tumors in the stomach and MEN1 syndrome, treatment may also include:
- Surgery (resection) to remove tumors in the duodenum (first part of the small intestine, that connects to the stomach).
- Hormone therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Neuroendocrine Tumors in the Small Intestine
For information about the treatments listed below, see the Treatment Option Overview section.
It is not clear what the best treatment is for gastrointestinal (GI) neuroendocrine tumors in the duodenum (first part of the small intestine, that connects to the stomach). Treatment may include the following:
- Endoscopic surgery (resection) for small tumors.
- Surgery (local excision) to remove slightly larger tumors.
- Surgery (resection) to remove the tumor and nearby lymph nodes.
Treatment of GI neuroendocrine tumors in the jejunum (middle part of the small intestine) and ileum (last part of the small intestine, that connects to the colon) may include the following:
- Surgery (resection) to remove the tumor and the membrane that connects the intestines to the back of the abdominal wall. Nearby lymph nodes are also removed.
- A second surgery to remove the membrane that connects the intestines to the back of the abdominal wall, if any tumor remains or the tumor continues to grow.
- Hormone therapy.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Neuroendocrine Tumors in the Appendix
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of gastrointestinal (GI) neuroendocrine tumors in the appendix may include the following:
- Surgery (resection) to remove the appendix.
- Surgery (resection) to remove the right side of the colon including the appendix. Nearby lymph nodes are also removed.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Neuroendocrine Tumors in the Colon
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of gastrointestinal (GI) neuroendocrine tumors in the colon may include the following:
- Surgery (resection) to remove part of the colon and nearby lymph nodes, in order to remove as much of the cancer as possible.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Neuroendocrine Tumors in the Rectum
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of gastrointestinal (GI) neuroendocrine tumors in the rectum may include the following:
- Endoscopic surgery (resection) for tumors that are smaller than 1 centimeter.
- Surgery (resection) for tumors that are larger than 2 centimeters or that have spread to the muscle layer of the rectal wall. This may be either:
It is not clear what the best treatment is for tumors that are 1 to 2 centimeters. Treatment may include the following:
- Endoscopic surgery (resection).
- Surgery (resection) to remove part of the rectum.
- Surgery (resection) to remove the anus, the rectum, and part of the colon through an incision made in the abdomen.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Metastatic Gastrointestinal Neuroendocrine Tumors
For information about the treatments listed below, see the Treatment Option Overview section.
Distant metastases
Treatment of distant metastases of gastrointestinal (GI) neuroendocrine tumors is usually palliative therapy to relieve symptoms and improve quality of life. Treatment may include the following:
- Surgery (resection) to remove as much of the tumor as possible.
- Hormone therapy.
- Radiopharmaceutical therapy.
- External radiation therapy for cancer that has spread to the bone, brain, or spinal cord.
- A clinical trial of a new treatment.
Liver metastases
Treatment of cancer that has spread to the liver may include the following:
- Surgery (local excision) to remove the tumor from the liver.
- Hepatic artery embolization.
- Cryosurgery.
- Radiofrequency ablation.
- Liver transplant.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
Treatment of Recurrent Gastrointestinal Neuroendocrine Tumors
For information about the treatments listed below, see the Treatment Option Overview section.
Treatment of recurrent gastrointestinal (GI) neuroendocrine tumors may include the following:
- Surgery (local excision) to remove part or all of the tumor.
- A clinical trial of a new treatment.
Use our clinical trial search to find NCI-supported cancer clinical trials that are accepting patients. You can search for trials based on the type of cancer, the age of the patient, and where the trials are being done. General information about clinical trials is also available.
To Learn More About Gastrointestinal Neuroendocrine Tumors
For more information from the National Cancer Institute about gastrointestinal neuroendocrine tumors, see the following:
For general cancer information and other resources from the National Cancer Institute, visit:
About This PDQ Summary
About PDQ
Physician Data Query (PDQ) is the National Cancer Institute's (NCI's) comprehensive cancer information database. The PDQ database contains summaries of the latest published information on cancer prevention, detection, genetics, treatment, supportive care, and complementary and alternative medicine. Most summaries come in two versions. The health professional versions have detailed information written in technical language. The patient versions are written in easy-to-understand, nontechnical language. Both versions have cancer information that is accurate and up to date and most versions are also available in Spanish.
PDQ is a service of the NCI. The NCI is part of the National Institutes of Health (NIH). NIH is the federal government’s center of biomedical research. The PDQ summaries are based on an independent review of the medical literature. They are not policy statements of the NCI or the NIH.
Purpose of This Summary
This PDQ cancer information summary has current information about the treatment of adult gastrointestinal neuroendocrine tumors. It is meant to inform and help patients, families, and caregivers. It does not give formal guidelines or recommendations for making decisions about health care.
Reviewers and Updates
Editorial Boards write the PDQ cancer information summaries and keep them up to date. These Boards are made up of experts in cancer treatment and other specialties related to cancer. The summaries are reviewed regularly and changes are made when there is new information. The date on each summary ("Updated") is the date of the most recent change.
The information in this patient summary was taken from the health professional version, which is reviewed regularly and updated as needed, by the PDQ Adult Treatment Editorial Board.
Clinical Trial Information
A clinical trial is a study to answer a scientific question, such as whether one treatment is better than another. Trials are based on past studies and what has been learned in the laboratory. Each trial answers certain scientific questions in order to find new and better ways to help cancer patients. During treatment clinical trials, information is collected about the effects of a new treatment and how well it works. If a clinical trial shows that a new treatment is better than one currently being used, the new treatment may become "standard." Patients may want to think about taking part in a clinical trial. Some clinical trials are open only to patients who have not started treatment.
Clinical trials can be found online at NCI's website. For more information, call the Cancer Information Service (CIS), NCI's contact center, at 1-800-4-CANCER (1-800-422-6237).
Permission to Use This Summary
PDQ is a registered trademark. The content of PDQ documents can be used freely as text. It cannot be identified as an NCI PDQ cancer information summary unless the whole summary is shown and it is updated regularly. However, a user would be allowed to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks in the following way: [include excerpt from the summary].”
The best way to cite this PDQ summary is:
PDQ® Adult Treatment Editorial Board. PDQ Gastrointestinal Neuroendocrine Tumors Treatment. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: /types/gi-neuroendocrine-tumors/patient/gi-neuroendocrine-treatment-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389212]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use in the PDQ summaries only. If you want to use an image from a PDQ summary and you are not using the whole summary, you must get permission from the owner. It cannot be given by the National Cancer Institute. Information about using the images in this summary, along with many other images related to cancer can be found in Visuals Online. Visuals Online is a collection of more than 3,000 scientific images.
Disclaimer
The information in these summaries should not be used to make decisions about insurance reimbursement. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s E-mail Us.
Updated: